
What is Parkinson’s Disease?
Parkinson’s disease (PD) is a type of neurologic movement disorder, affecting the brain and causing difficulty with movements, or motor symptoms.
It is characterized by its most common motor symptoms — tremors (a form of rhythmic shaking), stiffness or rigidity of the muscles, and slowness of movement (called bradykinesia) — but also manifests in non-motor symptoms including sleep problems, constipation, anxiety, depression, and fatigue, among others, which can be present well before any visible motor symptoms. It is a chronic and progressive condition, meaning that the symptoms become worse over time and can affect the ability to perform common, daily activities.
Who does the disease affect?
There are an estimated 1 million people in the U.S. living with Parkinson’s disease and more than 10 million people worldwide. Most people who develop the symptoms of Parkinson’s disease do so sometime after the age of 50, but Parkinson’s disease can affect younger persons as well. Approximately 10% of Parkinson’s diagnoses occur before age 50—these diagnoses are called Young Onset (or Early Onset) Parkinson’s disease.
Understanding Parkinson’s Disease

Parkinson’s Disease: The Essentials
If you’re new to Parkinson’s disease and would like a good overview to help you better understand the disease, please view our Parkinson’s Disease: The Essentials presentation. It’s a great place to get started with reliable and concise information.
Learn More About Parkinson’s Disease
Symptoms of Parkinson’s
Parkinson’s disease symptoms vary widely among individuals, presenting a unique combination of motor and non-motor signs. The hallmark symptoms include tremors, stiffness, and slowness of movement, impacting daily activities and quality of life. Additionally, non-motor symptoms such as sleep disturbances, mood changes, and cognitive challenges are increasingly recognized for their significant impact. Early identification and management of these symptoms are crucial for improving patient outcomes.
Causes of Parkinson’s
Understanding the causes of Parkinson’s disease involves exploring a complex interplay of genetic and environmental factors. Research suggests that a combination of genetic predispositions and environmental exposures (such as pesticides and solvents) may contribute to the disease’s onset, although in most cases it is unlikely to know the specific cause(s) of someone’s PD. Ongoing research studies aim to uncover specific genetic markers and environmental risks, offering hope for targeted treatments and prevention strategies.
Potential causes and risk factors
How does Parkinson’s disease affect the brain?
What makes Parkinson’s disease distinctive is that cell loss occurs in various brain regions, including the substantia nigra (sub-STAN-she-uh NYE-gruh). The nerve cells, or neurons, in this region appear dark under a microscope (substantia nigra is Latin for “black substance”).

These dark neurons produce a neurotransmitter (a chemical messenger that allows neurons to communicate) called dopamine, which helps to regulate movement. When the cells of the substantia nigra die, they no longer produce dopamine, leading to challenges with movement. This loss of dopamine is the reason that many treatments for Parkinson’s disease are intended to increase dopamine levels in the brain.
In addition to decreases in dopamine and the cells that make dopamine, you might also read or hear about alpha-synuclein (AL-fa-sin-NUKE-lee-un). Alpha-synuclein appears to play a variety of roles in the healthy brain, but in PD it clumps up in various types of nerve cells in the brain including the cells of the substantia nigra. These abnormal accumulations of alpha synuclein are called Lewy (LOO-ee) bodies. Researchers believe that alpha-synuclein build-up contributes to the death of these neurons, and are therefore a key element in the development of PD. Research is currently focused on ways to decrease the buildup of alpha-synuclein as potential treatments for PD. Learn more about APDA research initiatives here.
Diagnosing Parkinson’s disease
Currently, Parkinson’s disease (PD) diagnosis is based on a visual clinical exam done by a doctor (ideally a neurologist or movement disorder specialist) in their office. This means that motor symptoms such as tremor, stiffness and slowness must be apparent before a diagnosis is made by the neurologist. An imaging test called a DaTscan is available for certain clinical situations when the diagnosis is not clear based on clinical exam alone. However, advances in the development of biomarkers are poised to change how PD is diagnosed and potentially allow for diagnosis earlier than when motor symptoms develop.
How Parkinson’s disease is diagnosed
Treatment & Medication
As of today, there is no cure for Parkinson’s disease. But there are many ways in which the disease can be treated to make symptoms more manageable. Treatment for the disease is tailored to each individual’s symptoms and may include medication, lifestyle changes, and sometimes surgery. The goal is always to manage symptoms effectively and improve quality of life.
Learn about the range of treatment options
Living with Parkinson’s
Following diagnosis, it’s essential to focus on symptom improvement and maintaining an active, positive lifestyle. This involves regular exercise, a healthy diet, exploring various medication and treatment options, and building a supportive healthcare team. It is also important to take care of your emotional wellbeing through support groups, therapy, social activities, and other efforts that will provide opportunities to talk about your PD with others who understand what you’re going through. Effective management of PD symptoms can greatly enhance quality of life. For more guidance on living well with PD, including practical tips and resources, follow the link below.
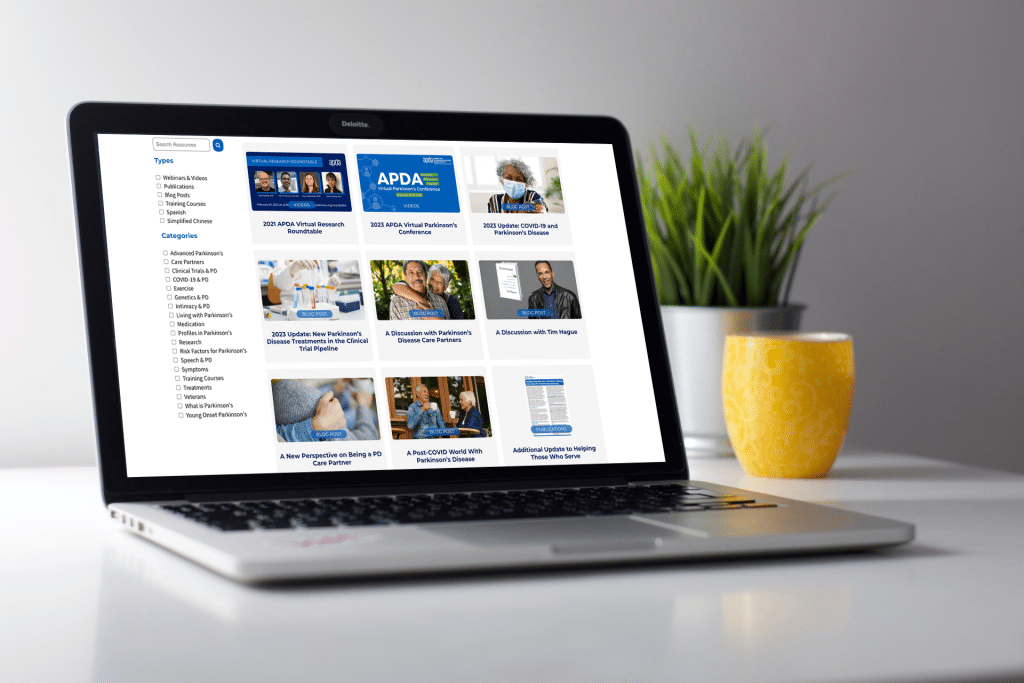
Explore Our Parkinson’s Resource Library
Whether you are living with PD, caring for someone with PD, or are just looking for information, check out our new resource library to see articles, videos, webinars, and more in-depth information about Parkinson’s disease.
